
Quick Links
Resources
About MyEczemaTeam
Powered By





| KEY TAKEAWAYS: |
|
Eczema is a chronic, inflammatory skin condition where people develop dry, itchy, and scaly rashes. Eczema is not contagious. People with eczema, especially atopic dermatitis, have a less effective skin barrier that leads to dry skin and lets in irritants that trigger an abnormal reaction from the immune system. Read more about eczema.
Eczema can begin as early as the first few months of life – upwards of 90 percent of people with eczema develop the condition before age 5. About half of those with moderate or severe eczema also experience food allergies, asthma, and allergic rhinitis – commonly called hay fever. Many parents of young children with eczema are told they will “outgrow” eczema, sometimes by health care providers. While this may be the case for some children, many people continue to experience eczema as a chronic condition during adolescence and throughout their lives. The areas of skin affected by eczema can change from infancy to adolescence.
Beyond the physical discomforts of eczema, symptoms like itchy or scaly skin can negatively impact people’s emotional well-being and social life. Sleep is affected, as well as performance in school. Social isolation, stigma, and bullying are commonly reported by children and teens with eczema. These negative experiences can contribute to mental health problems in some young people.
A study of approximately 3,550 18- and 19-year-olds found that mental health problems were more prevalent in teens (especially girls) with eczema than those without.
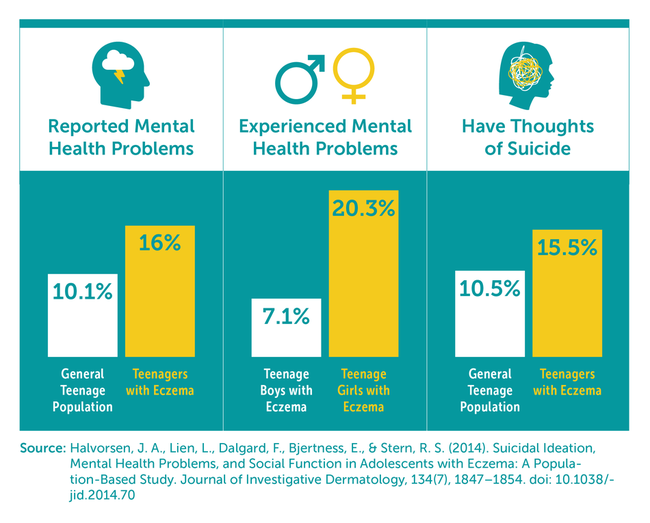
While it’s common for teens to struggle with emotional difficulties related to eczema, many are able to become more accepting of their condition and grow in self-confidence over time. Speaking with a therapist or other mental health provider can help you manage difficult emotions related to eczema. If you have thoughts of self-harm, call 911 or the National Suicide Prevention Lifeline at 800-273-8255.
Sticking to a regular eczema treatment routine as prescribed by a doctor is the best way to manage eczema over the long term, minimize flare-ups, and avoid infections. Sticking to a routine can be tricky for lots of reasons, especially for teens who are busy with school or other activities. Applying lotions, moisturizers, or treatments such as topical corticosteroids correctly can be time-consuming, and remembering to take medications can be challenging if you’re not used to a medication routine. It can also be frustrating when treatments don’t appear to be making a difference, or when it’s unclear why symptoms are getting better or worse.
Alongside the everyday challenges and frustrations of following a treatment routine, teens often don’t have enough information about eczema treatment. As responsibility for eczema care shifts away from parents to teens, they don’t always receive enough information or support from their doctors to make a smooth transition. The result of this knowledge gap can be improvised treatment routines that differ from doctor recommendation

One of the best things to do is take steps to be an active participant in your eczema care. A first action can be talking to your doctor about your treatment plan to ensure you understand all of the steps, what to expect, and how to know if it’s successful. It’s also important to remember that eczema is a complex and chronic skin disease that is not your fault, although there are things you can do to improve it. There is no quick fix. Managing eczema requires incorporating treatment and self-care practices into your daily habits.
Making lifestyle adjustments to manage eczema can be difficult for everyone, especially teens and young adults. At an age when many people are exploring different modes of self-expression, it can be hard to accept that aspects of personal care such as hair color, fragrances, makeup, or jewelry may trigger eczema. Late nights and erratic sleep schedules, common among young adults, can worsen skin problems. Sticking to a good skin care regimen every day may seem burdensome at first, but over time it will just feel normal. Adopting a daily routine that protects your skin can help it stay its healthiest.

|
Showering and BathingLong, hot showers or baths may be relaxing, but they can damage the skin barrier of people with eczema. Shorter — five to 10-minute — showers or baths in lukewarm water are better for the skin. Wash your body with a gentle, fragrance-free, non-soap cleanser and avoid harsh scrubbing.7 Wash your hair with fragrance-free shampoos and conditioners. Try your best to limit the amount of shampoo or conditioner that touches your skin — you can wash your hair in the sink instead of the shower or bath to avoid product touching your skin. Once out of the shower or bath, gently pat your skin so it’s mostly but not completely dry — avoid harsh rubbing with a towel. Apply a generous amount of moisturizer within three minutes of toweling off. Wait for the moisturizer to absorb into the skin before getting dressed. |
|
|
|
|
|
|
|
|
MyEczemaTeam is the social network for people with eczema and their loved ones. Here, more than 36,000 members from around the world come together to swap stories and advice, discuss daily life with eczema, and meet others who understand the diagnosis.
Do you have tips for managing eczema? Share your experience in the comments below or by posting on MyEczemaTeam.
A MyEczemaTeam Member
My dermatologist says their is something called Polymorphic light Eruption. I get itchy bumps when I go out in spring summer from sunlight and heat.